The opioid crisis in Appalachia remains a profound public health challenge, exerting an outsized impact on the region compared to other parts of the United States. While national efforts to address opioid misuse and overdose deaths have demonstrated some progress, Appalachia continues to experience elevated rates of mortality related to opioids, reflecting the complexity of the epidemic in this region. The crisis has transformed over time, moving from prescription opioid misuse to a landscape dominated by illicit synthetic opioids such as fentanyl, alongside the increasing use of other substances, including methamphetamine. This evolution of the crisis has intensified health risks, particularly in rural areas, where access to treatment and preventive services is often limited.
Current Status and Trends
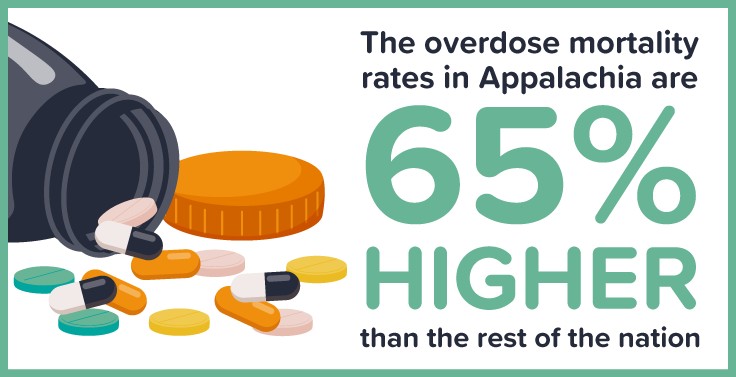
Overdose rates in Appalachia remain alarmingly high. In 2022, individuals aged 25 to 54 experienced overdose mortality rates 64 percent higher than those observed in other parts of the country. This disparity highlights the enduring vulnerability of Appalachian communities and the intensity of the crisis within the region. The heightened prevalence of overdose deaths is closely linked to the rise of synthetic opioids, particularly fentanyl, which presents unprecedented dangers due to its potency. Fentanyl is often mixed into other drugs without the knowledge of users, creating highly unpredictable supply chains and increasing the likelihood of fatal overdoses.
Alongside the fentanyl epidemic, polysubstance use has emerged as a significant concern. Individuals frequently consume multiple substances simultaneously, combining opioids with stimulants such as methamphetamine. This pattern of use elevates the risk of overdose, complicates treatment strategies, and poses challenges for public health interventions. Polysubstance use reflects broader shifts in substance availability and use patterns in Appalachia, and it underscores the need for comprehensive strategies that address multiple substances rather than focusing exclusively on opioids.
Rural disparities continue to define the opioid crisis in Appalachia. Rural counties consistently report the highest opioid-related death rates, often exceeding those of urban or metropolitan areas within the region. Geographic isolation, long travel distances to healthcare facilities, and limited availability of specialized treatment services amplify the risks faced by residents in rural communities. These structural challenges interact with broader socioeconomic conditions, creating an environment where overdose risk and barriers to treatment converge.
Key Challenges
Socioeconomic factors play a critical role in perpetuating the opioid crisis in Appalachia. High rates of poverty, limited educational opportunities, and constrained access to stable employment contribute to conditions that increase vulnerability to substance use disorder. Communities experiencing economic distress often see elevated rates of opioid misuse and overdose, reflecting the strong connection between social and economic wellbeing and public health outcomes. The economic challenges in Appalachia also impact workforce stability, community resources, and the ability of local governments to respond effectively to the epidemic.
Barriers to treatment present additional obstacles for individuals seeking help. Access to healthcare professionals specializing in substance use treatment remains limited across much of the region. Many counties lack specialized treatment facilities, and the high cost of care can place treatment out of reach for residents. Transportation difficulties further compound these challenges, particularly in rural areas where individuals may need to travel long distances to reach treatment programs. These barriers limit the reach of evidence-based interventions and slow efforts to reduce overdose mortality.
Stigma surrounding substance use disorder and harm reduction strategies further complicates response efforts. In small, rural communities, individuals may encounter social and cultural resistance to seeking treatment, which can delay or prevent engagement with healthcare services. Misunderstandings about substance use disorder contribute to a lack of support for harm reduction initiatives, including the distribution of naloxone, a life-saving medication that reverses opioid overdoses. The persistence of stigma undermines community resilience and the effectiveness of public health interventions.
Limited resources in Appalachian counties also hinder efforts to combat the opioid epidemic. Local governments often operate with fewer per capita resources than urban areas, constraining their capacity to implement comprehensive prevention, treatment, and recovery programs. Funding constraints affect the availability of trained personnel, infrastructure for treatment, and the development of community-based initiatives. In this context, leveraging regional partnerships and external funding sources becomes essential for sustaining effective public health responses.
Response Efforts
Community-based solutions have emerged as a central strategy in addressing the opioid crisis in Appalachia. Collaborative initiatives that engage public, private, and non-profit sectors aim to create sustainable support networks for individuals affected by substance use disorder. These solutions recognize the importance of local knowledge, community trust, and culturally appropriate interventions in achieving meaningful outcomes. By building partnerships across sectors, communities can expand access to services, improve resource allocation, and strengthen resilience against the epidemic.
The Appalachian Regional Commission (ARC) has played a critical role in funding and supporting regional initiatives. Programs such as the Investments Supporting Partnerships In Recovery Ecosystems (INSPIRE) program work to establish community-based recovery systems tailored to the needs of local populations. In addition, opioid abatement settlement funds provide opportunities for scaling evidence-based interventions, supporting prevention efforts, and enhancing access to treatment. These investments reflect a recognition that long-term solutions require not only medical interventions but also systemic support for communities impacted by substance use.
Harm reduction strategies have gained increasing attention as an effective approach to reducing overdose mortality. Public health organizations collaborate with state and local officials to expand services, including the distribution of naloxone, syringe exchange programs, and educational initiatives designed to reduce the harms associated with substance use. By emphasizing practical measures that save lives and reduce health risks, harm reduction initiatives complement broader treatment and recovery efforts. These strategies are particularly important in rural communities where medical infrastructure may be limited, and immediate access to emergency care can be challenging.
Efforts to build recovery ecosystems aim to address the social determinants of health that contribute to substance use disorder. Comprehensive recovery approaches extend beyond medical treatment to include support for housing, employment, legal aid, and social services. By addressing underlying social and economic factors, recovery ecosystems enhance the capacity of individuals to sustain long-term recovery and reintegration into their communities. This holistic approach acknowledges the complex interplay of health, social, and economic conditions in shaping outcomes for individuals and families affected by substance use disorder.
Despite some evidence of national progress in slowing the rate of increase in overdose deaths, the situation in Appalachia remains urgent. The combination of high overdose rates, rural disparities, polysubstance use, and socioeconomic challenges creates a uniquely challenging environment for public health intervention. Ongoing efforts focus on expanding access to evidence-based treatment, scaling harm reduction services, and addressing root causes that contribute to vulnerability. Investments in community-based solutions and recovery ecosystems demonstrate the potential for sustainable progress, provided that initiatives continue to receive adequate support and funding.
Looking forward, the region faces opportunities to strengthen the response to the opioid crisis. Enhancing coordination among public health agencies, community organizations, and healthcare providers can improve the efficiency and reach of interventions. Data-driven approaches allow for more precise identification of high-risk populations, enabling targeted prevention and treatment strategies. Education and awareness campaigns can reduce stigma, promote harm reduction practices, and encourage early engagement with treatment services. By integrating medical, social, and economic interventions, communities can build resilience against the ongoing challenges posed by the opioid epidemic.
Investments in workforce development, education, and economic opportunity are essential components of a comprehensive strategy. By addressing structural inequalities and expanding pathways for social and economic mobility, communities can reduce underlying risk factors that contribute to substance misuse. This approach reinforces the importance of viewing the opioid crisis not solely as a medical problem but as a multidimensional public health challenge shaped by social and economic conditions.
In conclusion, the opioid crisis in Appalachia remains a serious and complex public health issue, disproportionately affecting the region compared to the rest of the United States. Elevated overdose mortality rates, driven primarily by synthetic opioids such as fentanyl, continue to pose significant health risks, particularly in rural counties. Polysubstance use, socioeconomic disparities, barriers to treatment, and stigma create additional challenges that complicate the response to the epidemic. Despite national progress, the urgency of the situation in Appalachia demands sustained attention, comprehensive strategies, and robust investments in both public health and social support systems. Community-based initiatives, harm reduction services, recovery ecosystems, and targeted funding represent critical tools for mitigating the crisis and supporting affected populations. By addressing the opioid epidemic through a combination of medical, social, and economic interventions, Appalachia has the potential to achieve meaningful improvements in public health outcomes, reduce overdose mortality, and strengthen the resilience of its communities in the face of ongoing challenges.
-Tim Carmichael
Leave a comment