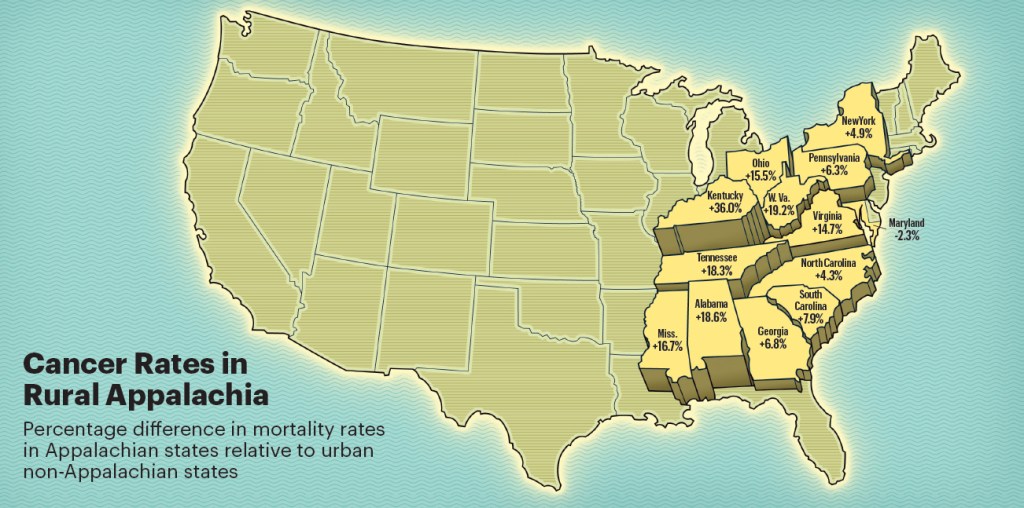
Cancer continues to represent one of the greatest health challenges in the United States, claiming hundreds of thousands of lives each year despite advances in medical technology and treatment. While the nation overall has experienced encouraging declines in both cancer incidence and mortality over recent decades, the story looks very different when focusing on Appalachia. Across this vast region that spans 13 states and stretches from southern New York into northern Mississippi, communities face disproportionately higher cancer burdens compared to the rest of the country. The data is both striking and sobering: mortality rates in Appalachia as a whole stand about 10 percent higher than the national average, while in Central Appalachia, a subregion encompassing parts of Kentucky, West Virginia, Virginia, and Tennessee, the mortality rate rises to an alarming 32 percent higher than the rest of the nation.
Elevated cancer mortality represents only part of the picture. The Appalachian region also demonstrates higher rates of cancer diagnoses compared to non-Appalachian areas. Between 2017 and 2021, cancer incidence was 5.6 percent higher in Appalachia than in the rest of the country. This dual challenge both a greater likelihood of being diagnosed and a greater likelihood of dying from the disease illustrates the scale of health inequities present in these communities. What makes this reality particularly concerning is the persistence of disparities, even as progress occurs nationally. While cancer mortality has declined overall across the United States, these declines have occurred more slowly in states like Kentucky, with the lag most pronounced in its Appalachian counties. Research from the University of Kentucky highlights how improvements in treatment and early detection have reached some areas much more effectively than others, leaving certain Appalachian communities trapped in a cycle of delayed progress.
Explaining why Appalachia carries such a heavy cancer burden requires attention to a combination of structural, economic, behavioral, and environmental factors. A central challenge is access to healthcare. Many communities within the region are rural and geographically isolated, with fewer physicians, clinics, and hospitals serving wide geographic areas. When healthcare services exist, they are often limited in scope, forcing residents to travel long distances for specialized care such as oncology treatment. For families with limited resources, inadequate transportation options, or tight work schedules, these distances pose formidable obstacles. Insurance status compounds these difficulties. Appalachia has higher proportions of individuals who are uninsured or underinsured compared to the national average, meaning even when services are available, they may remain financially out of reach for many residents.
This access gap directly influences cancer outcomes through delayed diagnosis and treatment. Screening for cancers such as breast, colorectal, and cervical cancers has proven critical for detecting disease early, when interventions have a greater chance of success. Nationally, major campaigns have expanded awareness and increased participation in screening programs, contributing to mortality declines. Yet in Appalachia, screening rates remain consistently lower than in other regions. Lower screening rates mean cancers are often discovered at later stages, when options for treatment are fewer, less effective, and more costly. This reality connects directly to the higher mortality rates documented across the region.
Economic hardship is another central driver of disparities. Appalachia has long faced economic challenges tied to industrial shifts, resource extraction, and limited job diversification. Persistent poverty in many counties shapes both daily life and health outcomes. Higher poverty rates correlate with reduced access to nutritious food, safe housing, and consistent healthcare. The stress of financial insecurity also influences health behaviors, creating environments where rates of smoking and obesity are elevated compared to national averages. These behaviors are closely linked to multiple cancer types, further increasing incidence and mortality. For example, smoking remains particularly prevalent in Central Appalachia, contributing significantly to lung cancer rates that exceed national averages.
Historical and occupational exposures add yet another layer. Coal mining, central to the history and economy of many Appalachian communities, has left a complicated legacy for health. Long-term exposure to coal dust and related hazards has been associated with respiratory diseases and potential cancer risks. While mechanization and regulation have reduced direct exposure for workers in recent decades, the long shadow of occupational hazards continues to affect older generations and, in some cases, environmental quality in mining regions. Families in communities with long histories of coal mining often live near abandoned sites or areas where environmental contamination remains a concern, further increasing risks.
Cultural and social dynamics also influence outcomes. Appalachia is rich in cultural traditions, resilience, and strong community networks, yet these same close-knit structures sometimes contribute indirectly to health disparities. Attitudes toward preventive healthcare, for example, can reflect skepticism of outside institutions, hesitancy toward medical procedures, or fatalistic views of illness. In communities where cancer has touched nearly every family, some residents may perceive diagnosis as an unavoidable outcome rather than a condition that can be mitigated through screening and early intervention. These perceptions can delay decisions to seek care, reinforcing cycles of late diagnosis and poorer outcomes.
The persistence of disparities, even amid nationwide progress, demonstrates how entrenched these challenges have become. For instance, in Kentucky overall, significant investments have been made to address cancer through research and outreach. Yet when researchers analyze outcomes specifically in Appalachian counties, they find that improvements occur at a slower pace, widening the gap between Appalachia and non-Appalachian areas. This illustrates how broad national or even statewide initiatives may fail to reach their full potential without strategies tailored to the unique circumstances of Appalachian communities.
Addressing cancer disparities in Appalachia requires multi-faceted strategies that go beyond traditional healthcare delivery. Expanding access to preventive care is essential, which means increasing the availability of clinics, strengthening telehealth infrastructure, and ensuring affordability of services for uninsured or underinsured residents. Community-based outreach programs tailored to local cultures and values can improve trust and encourage greater participation in screening programs. Policies aimed at reducing poverty and improving education levels can indirectly support better health behaviors, creating conditions that lower cancer risk over time. Addressing environmental and occupational health risks also remains critical, ensuring that communities historically tied to industries such as coal mining do not continue to bear disproportionate burdens of exposure-related disease.
Equally important is the role of research and advocacy. Institutions such as the University of Kentucky’s Markey Cancer Center and other regional research hubs have invested in studying Appalachian health disparities, raising awareness and developing targeted interventions. Partnerships between universities, healthcare providers, and community organizations can foster programs that resonate with local populations and address barriers more effectively than one-size-fits-all approaches. For example, mobile mammography units or local patient navigation programs can make cancer screening more accessible while also helping individuals navigate insurance paperwork, transportation logistics, and appointment scheduling.
Ultimately, reducing cancer disparities in Appalachia depends on bridging structural inequities while fostering trust and engagement within communities. The statistics 10 percent higher mortality across Appalachia, 32 percent higher mortality in Central Appalachia, 5.6 percent higher incidence between 2017 and 2021 are not mere abstractions. They represent families losing loved ones too soon, communities struggling with grief, and entire regions experiencing a burden of disease heavier than elsewhere in the nation. By recognizing the unique challenges faced in Appalachia and committing resources to targeted solutions, it is possible to change this trajectory.
Cancer disparities in Appalachia reflect more than health issues alone; they reflect broader patterns of inequality that intersect with geography, economics, history, and culture. While progress has been slower here than in other regions, change is not beyond reach. With sustained commitment, focused interventions, and respect for the voices of Appalachian communities, the next decades can see more equitable outcomes. Reducing the cancer burden in Appalachia would not only improve lives in the region itself, but it would also strengthen the nation’s broader fight against cancer by ensuring no community is left behind.
-Tim Carmichael
Leave a comment