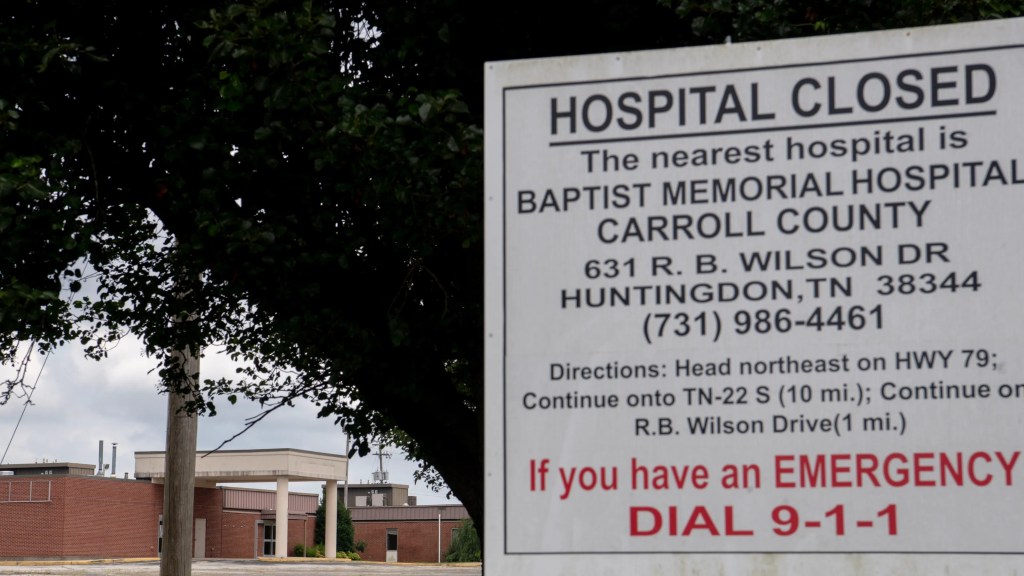
As the autumn of 2025 unfolds, Appalachia finds itself facing an escalating rural health crisis. Across this vast region, stretching from New York through Pennsylvania and down to Mississippi, hospitals and clinics continue to shutter or scale back services. While national media has covered hospital closures broadly, no official, comprehensive tally exists specifically for the Appalachian region this year. Advocacy groups, local journalists, and nonprofit organizations have pieced together the most visible losses, yet the true scope remains unclear. Even without a formal total, evidence shows that closures and service cuts have intensified in Appalachia throughout 2025.
Communities throughout the region are confronting harsh realities tied directly to financial pressure. Federal Medicaid reductions, compounded by long-standing structural disadvantages, have accelerated the decline of rural hospitals. For residents of Appalachia, the consequences are measured in longer drives to seek care, dwindling access to essential services, and rising fear about what the future holds for their families and towns.
Tennessee provides a sobering illustration of the problem. Already recognized as the state with the highest rate of rural hospital closures per capita in the United States, Tennessee remains on the front lines of this worsening trend. In 2025, reports indicate that nine rural hospitals in Tennessee are considered “at risk” of either shutting their doors entirely or slashing services. The threat looms large due to potential Medicaid reductions linked to the federal legislation passed earlier this year. For communities in places like west Tennessee or the Cumberland Plateau, the prospect of losing the only nearby emergency room raises concerns about life-threatening delays in urgent care.

Pennsylvania, often thought of as better resourced than southern Appalachian states, is facing its own acute challenges. The Appalachia Funders Network reported in August that nine rural hospitals in Pennsylvania are at immediate risk of closure. Of these, five were specifically named as vulnerable to Medicaid funding shifts. Such closures would have profound consequences for rural counties already struggling with physician shortages and limited specialty care. For residents of central and northern Pennsylvania, where mountainous terrain and winter storms can make travel treacherous, the loss of a hospital can mean far more than inconvenience. It can be a matter of survival.
The crisis is not confined to Tennessee and Pennsylvania. States including Kentucky, North Carolina, Virginia, Ohio, and West Virginia are also under threat. These states, all deeply rooted in the Appalachian region, face the same financial pressures that undermine sustainability for small rural hospitals. Federal Medicaid funding reductions, introduced through the One Big Beautiful Bill Act passed in 2025, are expected to cut billions of dollars in support for rural areas. Analysts have warned that the legislation will devastate Appalachia’s health care system, striking at the hospitals and clinics that sustain countless communities. Importantly, the cuts are structured so that they do not take effect until after the mid-term elections, which means many voters will only feel the full impact once they have already cast their ballots.
Financial instability is not a new issue for rural hospitals, yet the scale of distress in 2025 is striking. In February, the health care consulting firm Chartis released a report showing that a high percentage of rural hospitals across the country were operating on negative margins. In Appalachian states, the number of hospitals categorized as vulnerable was especially pronounced. The report warned that absent significant policy intervention, closures would continue at an alarming pace. For communities, negative margins mean hospitals struggle to cover even basic operating costs, leaving them unable to invest in upgrades, retain skilled staff, or expand services.

The closure crisis is not limited to complete shutdowns. Across Appalachia, many hospitals are responding to financial strain by reducing or eliminating critical services. Obstetric care is frequently among the first to go. Women in rural areas are increasingly forced to travel great distances for prenatal and delivery services, placing them at higher risk of complications. Pediatric care is another casualty, leaving families scrambling to find specialists for their children. Emergency departments may remain open in some facilities, yet without comprehensive inpatient support, their capacity to handle serious cases diminishes. The pattern represents a quiet erosion of access that does not always appear in closure tallies yet carries life-altering consequences for residents.
Tracking the true scope of closures in Appalachia is a complex undertaking. Hospitals and health systems often announce decisions on their own schedules, meaning there is no centralized real-time accounting of closures. Advocacy groups and journalists compile reports as they emerge, though these accounts can lag behind events on the ground. The absence of a unified, official tally makes it difficult for policymakers and communities to fully grasp the magnitude of the crisis as it unfolds. Frequently, the most authoritative figures are released retrospectively, long after closures have already reshaped access to care.
Further complicating matters is the distinction between full closure and conversion. Some hospitals do not shut down entirely, yet they discontinue inpatient care, transitioning instead to outpatient or emergency-only models. While these conversions technically preserve a facility’s presence in a community, they represent a profound reduction in available services. A hospital that no longer offers inpatient care cannot provide the same level of support for serious conditions, extended recovery, or specialized procedures. These conversions can be difficult to track, and while they may not appear in closure statistics, they represent a significant loss of capacity across Appalachia.
The consequences of these closures ripple far beyond the walls of the hospitals themselves. Local economies feel the blow immediately. Rural hospitals are often among the largest employers in their counties, and when they close, jobs vanish. The departure of skilled health professionals further accelerates population decline, as families seek opportunities and services elsewhere. For small towns already struggling with shrinking tax bases and aging populations, the loss of a hospital can push communities closer to economic collapse.
Health outcomes also reflect the toll. Rural residents already face higher rates of chronic illnesses such as diabetes, heart disease, and respiratory conditions. Reduced access to care compounds these challenges. When hospitals close or reduce services, preventive care often becomes harder to access, leading to worsening health over time. Delays in emergency care can mean the difference between recovery and tragedy. In this sense, the closure crisis in Appalachia is not only a matter of economics but also a question of life and death.
Advocacy organizations across the region continue to call for urgent policy action. They argue that rural hospitals should be supported as critical infrastructure, on par with roads and schools. In their view, sustaining health care access in rural America requires recognizing its role in community survival and development. The Appalachia Funders Network and similar groups emphasize that Medicaid funding serves as a lifeline for many hospitals. Reductions in this lifeline, they contend, risk devastating consequences for millions of residents. The One Big Beautiful Bill Act stands at the center of these concerns, as many see it as the single greatest threat to the survival of Appalachian hospitals in the modern era.
Community leaders, too, are sounding alarms. In many Appalachian towns, citizens are mobilizing to defend their local hospitals, organizing petitions, contacting legislators, and holding public forums. While such efforts sometimes succeed in delaying closures, they rarely reverse financial realities. Without structural changes to funding models, many hospitals remain in precarious positions. Grassroots action demonstrates the determination of residents to preserve their health care, yet it also underscores the desperation of communities left to fight for survival.
Looking ahead, the future of rural health care in Appalachia remains uncertain. Policymakers continue to debate the balance between controlling federal spending and ensuring equitable access to medical care. For communities across Appalachia, the stakes could not be higher. The trajectory of closures and service reductions in 2025 highlights the urgent need for solutions that stabilize rural hospitals, protect vulnerable populations, and recognize the unique challenges of serving geographically dispersed communities.
The crisis also forces a broader conversation about equity in American health care. Appalachia’s struggles mirror those in other rural regions, yet the depth of poverty and the scale of geographic isolation amplify the impact. As the nation considers its priorities, the question arises: what responsibility does society have to ensure that residents of rural areas receive timely, quality care? The answer will shape not only the future of Appalachia but also the broader fabric of American health care.
For now, residents across the Appalachian region continue to adapt to a shifting landscape of access. Families travel farther for care, hospitals cut vital services, and communities fight to keep their facilities afloat. Without immediate intervention, the crisis is likely to deepen, further isolating rural populations and straining already fragile systems. Appalachia’s story in 2025 is one of resilience amid decline, of communities striving to maintain their health care lifelines even as financial forces threaten to sever them. The outcome of this struggle will define the region’s health and vitality for decades to come.
-Tim Carmichael
Leave a comment